
Anyone who has suffered from jet lag or struggled after turning the clock forward or back an hour for daylight saving time knows all about what researchers call your biological clock, or circadian rhythm – the “master pacemaker” that synchronizes how your body responds to the passing of one day to the next.
This “clock” is made up of about 20,000 neurons in the hypothalamus, the area near the center of the brain that coordinates your body’s unconscious functions, like breathing and blood pressure. Humans aren’t the only beings that have an internal clock system: All vertebrates – or mammals, birds, reptiles, amphibians and fish – have biological clocks, as do plants, fungi and bacteria. Biological clocks are why cats are most active at dawn and dusk, and why flowers bloom at certain times of day.
Circadian rhythms are also essential to health and well-being. They govern your body’s physical, mental and behavioral changes over each 24-hour cycle in response to environmental cues like light and food. They’re why more heart attacks and strokes occur early in the morning. They’re also why mice that are missing their biological clocks age faster and have shorter lifespans, and people with a mutation in their circadian clock genes have abnormal sleep patterns. Chronic misalignment of your circadian rhythm with external cues, as seen in night-shift workers, can lead to a wide range of physical and mental disorders, including obesity, Type 2 diabetes, cancer and cardiovascular diseases.
In short, there is ample evidence that your biological clock is critical to your health. And chronobiologists like me are studying how the day-night cycle affects your body to better understand how you can modify your behaviors to use your internal clock to your advantage.
How biological rhythms affect your health
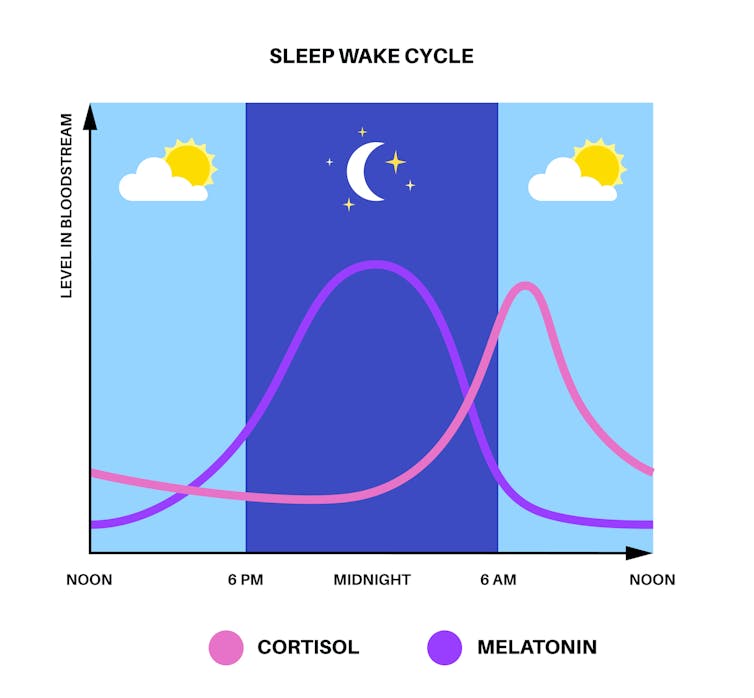
Your biological clock affects your health by regulating your sleep-wake cycles and fluctuations in blood pressure and body temperature. It does this primarily by syncing your endocrine system to environmental light-dark cycles so that certain hormones are released in certain amounts at certain times of day.
The pineal grand in your brain, for example, produces melatonin, a hormone that helps regulate sleep in response to darkness. Doctors advise reducing exposure to artificial blue light from electronic devices before bedtime because it can disrupt melatonin secretion and sleep quality.
Your circadian rhythm also affects your metabolism. Among other things, sleep helps you regulate leptin, a hormone that controls appetite. Your leptin levels fluctuate throughout the day according to a rhythm set by your circadian clock. Insufficient or irregular sleep can disrupt leptin production, which can make us hungrier and lead to weight gain.
In recent years, researchers have discovered even more ways your circadian clock can affect your health. For example, there is now research suggesting that eating at set times of day, or time-restricted feeding, can prevent obesity and metabolic diseases. Depression and other mood disorders may also be linked to dysfunctional circadian control that lead to changes in how your genes are expressed.
The time of day when you take your medicine can also affect how well it works and how severe any side effects might be. Likewise, your biological clock is a potential target for cancer chemotherapies and anti-obesity treatments.
And finally, even your personality might be shaped by whether your internal clock make you a “morning person” or a “night person.”
Getting the most out of exercise
Circadian clocks also provide a potential answer to when is the best time of day to maximize the benefits of physical exercise.
To study this, my colleagues and I collected blood and tissue samples from the brains, hearts, muscles, livers and fat of mice that exercised either before breakfast in the early morning or after dinner in the late evening. We used a tool called a mass spectrometer to detect approximately 600 to 900 molecules each organ produced. These metabolites served as real-time snapshots of how the mice responded to exercise at specific times of day.
We stitched these snapshots together to create a map of how exercise in the morning versus evening affected each of the mice’s different organ systems – what we called an atlas of exercise metabolism.

Using this atlas, we saw that time of day affects how each organ uses energy during exercise. For instance, we found that early morning exercise reduced blood glucose levels more than late evening exercise. Exercise in the late evening, however, allowed the mice to benefit from energy they stored from their meals and increased their endurance.
Of course, mice and humans have many differences along with their similarities. For one, mice are more active at night than during the day. Still, we believe that our findings could help researchers better understand how exercise affects your health and, if timed appropriately, can be optimized based on time of day to meet your personal health goals.
Getting along with your biological clock
I believe that the field of chronobiology is growing, and we will produce even more research providing practical applications and insights into health and well-being in the future.
In my own work, for example, a better understanding of how exercising at different times of day affects your body could help tailor exercise plans to maximize specific benefits for patients with obesity, Type 2 diabetes and other diseases.
There is still much to learn about how your circadian clock works. But in the meantime, there are some tried and true ways people can synchronize their internal clocks for better health. These include regular exposure to sunlight to trigger the endocrine system to produce vitamin D, staying active during the day so you fall asleep more easily at night and avoiding caffeine and reducing your exposure to artificial light before bedtime.![]()
Shogo Sato, Assistant Professor of Biology, Texas A&M University
This article is republished from The Conversation under a Creative Commons license.





